Improvements in mental health outcomes for individuals participating in Forward’s prison-led support programme

About Stepping Stones
Stepping Stones is a psychosocial intervention developed by Forward to support people using drugs or alcohol at harmful or dependent levels. First launched in 2012, the programme originally featured 20 sessions, designed to be delivered to groups of individuals in prison settings across 4 weeks. Stepping Stones uses Cognitive Behavioural Therapy (CBT)-based techniques specifically targeting areas identified as key skills for recovery:
- problem solving
- safe coping skills
- handling ‘triggers’ and ‘cravings’
- managing emotions such as anger
- managing mental health symptoms
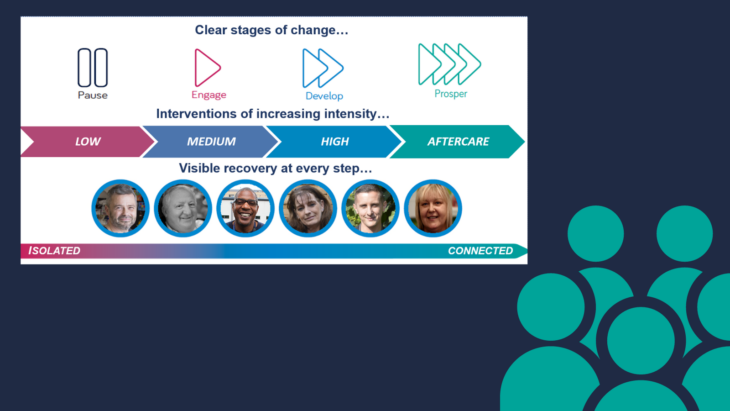
The programme is intended to prepare participants for more intensive treatment – categorised as an ‘Engage’ intervention within our integrated models of support, illustrated below, building skills and confidence to help people get started on their journey to recovery.
Stepping Stones re-launch 2021
As part of our commitment to continual service improvement, we undertook a comprehensive needs assessment of our substance misuse treatment offering in prison settings. This included analysis of current intervention efficacy and interviews and focus groups with our practitioners and service users. We identified an opportunity to reach more individuals by enhancing the flexibility of our Stepping Stones programme to reflect different regimes and lengths of sentence.
An updated Stepping Stones was co-produced and re-launched in 2021. It comprised 12 core sessions and 12 optional or additional sessions. New sessions were also developed, based on feedback:
- Understanding my emotions
- Substance use and mental health
- Substance use and offending
- Different types of drinking behavior (e.g. hazardous, harmful, dependent)
Evaluation

This new programme was internally evaluated in 2022 by the Research Team. Data from 194 Stepping Stones participants in 7 prison settings over the period September 2021-August 2022 were analysed to understand the efficacy of the new programme.
The majority of participants were Male (84%) with the Female participants (16%) reflecting our services in HMPs Downview and Send. Participants were majority white (71%); 146 (75%) of the cohort fell between the ages of 30-49. The cohort was considered reflective of the national treatment population, with the exception of our population having more diversity in ethnicity.
The majority of our service users fall into high drug-dependence (73%) and possible alcohol dependence (40%) categories on both the Substance Dependence Scale (SDS) and Alcohol Use Disorders Identification Test (AUDIT). The high number of individuals showing low risk alcohol use disorder scores (45%) often had alcohol as a secondary substance.
Results
The evaluation looked at completion rates and pre and post treatment psychometric scores for resilience, self-efficacy, and mental health (depression and anxiety). Where possible the results of the pre and post scores were assessed for their statistical significance (likelihood that the results are not due to chance). The mental health outcomes were later chosen for comparison against NHS mental health intervention outcomes, which dictates whether interventions which are developed to specifically target depression and anxiety are proven as effective in doing so.
Completion rates
“The evaluation showed that the programme was successfully completed by 89% of participants.”
The evaluation showed that the programme was successfully completed by 89% of participants, 14% higher than completion rates for the previous version of the programme, analysed in 2018. Increased completion was the primary aim of the re-launch of Stepping Stones, achieved despite COVID-19 and operational barriers to delivery.
Whilst not directly comparable this figure is also 57% higher than the national average completion rate for substance misuse treatment in a secure setting of 32% for 2020-21 (NDTMS, 2022).
Resilience
“The majority of individuals (53%) identified as having normal resilience at treatment end.”
Stepping Stones uses the Brief Resilience Scale (BRS) at programme start and end. The BRS assesses an individual’s perception of their ability to ‘bounce back’ or recover from stress.
On average, individuals who completed Stepping Stones increased their resilience scores from ‘pre’ to ‘post’. The majority of individuals (50%) showed low resilience at treatment start whereas the majority of individuals (53%) identified as having normal resilience at treatment end. Individuals considering themselves to have normal or high resilience at treatment end increased by around 30% overall, whereas individuals falling into low resilience decreased by around 30% overall.
Self-efficacy
“An 11% increase in their considerations of confidence to handle drink-taking situations.”
Stepping Stone uses the Drug/Alcohol Taking Confidence Questionnaire (D/ATCQ-8) at programme start and end. The D/ATCQ-8 measures an individual’s belief in their ability to manage or exert control in situations related to 50 drinking and drug taking scenarios.
Individuals who completed Stepping Stones showed, on average, an 11% increase in their considerations of confidence to handle drink-taking situations and a 16% increase in confidence toward drug-taking situations. Both of these results were found to be statistically significant and an improvement on the previous programmes scores.
Mental health
“60% of our substance misuse service users report having at least one mental health problem”
Finally, though Stepping Stones is not specifically designed as a mental health intervention (according to NICE categorisation) we measure common mental health symptomology, as 60% of our substance misuse service users report having at least one mental health problem. We use two validated tools, PHQ-9 for symptoms of depression, and GAD-7, which measures symptoms of anxiety.
Mental health (further analysis)
Depression
Individuals who successfully completed Stepping Stones showed, on average, a 24% decrease in mean scores for depression symptoms, with most decrease shown in individuals reporting higher severity of frequency of depression symptoms at intervention start. Individuals in the cohort meeting clinical ‘caseness’ (a score indicative of a formal depression diagnosis) reduced by 28% on average between pre and post data.
Anxiety
Individuals who successfully completed Stepping Stones showed, on average, a 20% decrease in mean scores for anxiety symptoms with most decrease shown in individuals reporting higher severity or frequency of anxiety symptoms at intervention start, a figure which improved from the 2018 evaluation of the historic Stepping Stones programme. Individuals in the cohort meeting clinical ‘caseness’ reduced by 27% on average between pre and post data.
Combined mental health (NHS outcomes)
Given the positive indicating results, we decided to measure the improvement in depression and anxiety scores against the more stringent NHS guidelines for what constitutes significant change in mental health symptomology. This level of evaluation combines two sets of scores (PHQ-9 and GAD-7) to identify whether the overall change is ‘clinically significant’ and likely to be sustained beyond the programme itself.
We found that 28% of individuals who completed Stepping Stones showed “reliable improvement” which indicates a significant improvement in their condition (anxiety and depression) following a course of treatment. The likelihood of achieving this outcome for mental health symptoms is an unexpected result from our analysis and a significant secondary benefit to our service users. This will be monitored in future evaluations where depression and anxiety scores in isolation indicate positive change.
Conclusion
The results of our evaluation show that the re-launched version of Stepping Stones has successfully reached a wider audience and achieved higher completion rates than the original version. The programme continues to build individuals’ resilience and confidence to assert themselves when faced with drug and alcohol taking situations and progress towards the next phase of their recovery. The secondary benefit identified of significantly improving mental health symptomology will continue to be monitored for its consistency and whether it aids in relieving pressure on secondary mental health services.
References
[1] HMPs Brixton, Coldingley, Downview, High Down, Send, Stoke Heath, The Mount